
Clinical Activity
Message from our Deputy Head of Clinical Affairs
Dr. Jonathan Gilleland
It is a privilege to serve the Department as your new Deputy Head of Strategic and Clinical Affairs and I look forward to working with, for, and alongside all of you in 2025. In the short time since starting in the role, I have already seen the Department’s vision of “Thriving Together” embodied in the willingness of its members to help out and support one another during this winter’s respiratory surge. As we face ongoing challenges of increasing patient complexity, growing populations, and evolving medical and technological advancements, it is our commitment to each other and our patients that will act as our greatest resource.
We will need your ongoing input and engagement on what types of expertise, resources, and innovations will be needed to address these challenges as we consider what pediatric medicine will look like in the future. As Winston Churchill once said: “The pessimist sees difficulty in every opportunity. The optimist sees opportunity in every difficulty”. I invite everyone to be optimists, and thank you for your resilience, teamwork, and kindness in serving your patients and our community.

Annie Ngu

Numbers are based off of the 2023-2024 fiscal year. Critical Care Visits include both NICU and PICU admissions. Emergency Department Visits are across both sites. Inpatient Visits are across both sites and exclude mental health and surgical admissions. Outpatient Visits do not include the thousands of children and teens by members who are community-based pediatricians.
ACH’s Commitment to Vaccine Excellence
Vaccine Confidence Toolkit
We developed the Vaccine Toolkit to assist healthcare providers in effectively facilitating vaccination discussions with patients. The toolkit incorporates virtual simulation games aimed at training healthcare professionals in conducting these conversations with confidence and expertise. These games are designed with varying focuses: some are vaccine-specific, such as those addressing RSV and influenza vaccines; others are population-specific, including a game tailored for immunocompromised patients; and several address situational challenges, such as vaccine refusal and the moral distress healthcare providers may experience during these interactions. The use of gamification enhances the educational experience, ensuring its relevance across diverse healthcare providers while introducing innovative methods for vaccine education.
In addition to the simulation games, the toolkit includes resources tailored for both pediatric and adult patients, with additional materials aimed at supporting immunocompromised individuals and pregnant patients. A recent addition to the toolkit is a patient-centered tool designed to measure the impact of vaccine-related conversations in clinical settings, offering valuable insights into the patient experience.
This initiative received funding through a grant from the Immunization Partnership Fund (PHAC) and was developed by a multidisciplinary team led by Dr. Cora Constantinescu, an ACH physician, along with the Department of Pediatrics Communications staff, and experts Dr. Eliana Castillo, Dr. Taj Jadavji, Dr. Alyssa Lip, Dr. Zahra Shajani, Dr. Otto Vanderkooi, and the AHS data analytics team under the leadership of Dr. Kovacs-Burns.
✎ Dr. Cora Constantinescu

Dr. Carrah Bouma
Annie Ngu
Revolutionizing Youth Mental Health Care
Peter Lougheed Centre's New Pediatric Med Psych Unit
Background
The Pediatric Med Psych (Medical Psychiatric) Unit opened in September 2024 at the Peter Lougheed Centre (PLC), introducing a new way to care for youth with both medical and mental health needs. After two years of planning and a generous $5 million donation from a private donor, the unit now offers 12 inpatient beds, including six of which are dedicated to patients needing both types of care. These beds were converted from our existing complement of 12 beds for the purpose of caring for this special population.
Guiding the Vision for Integrated Care
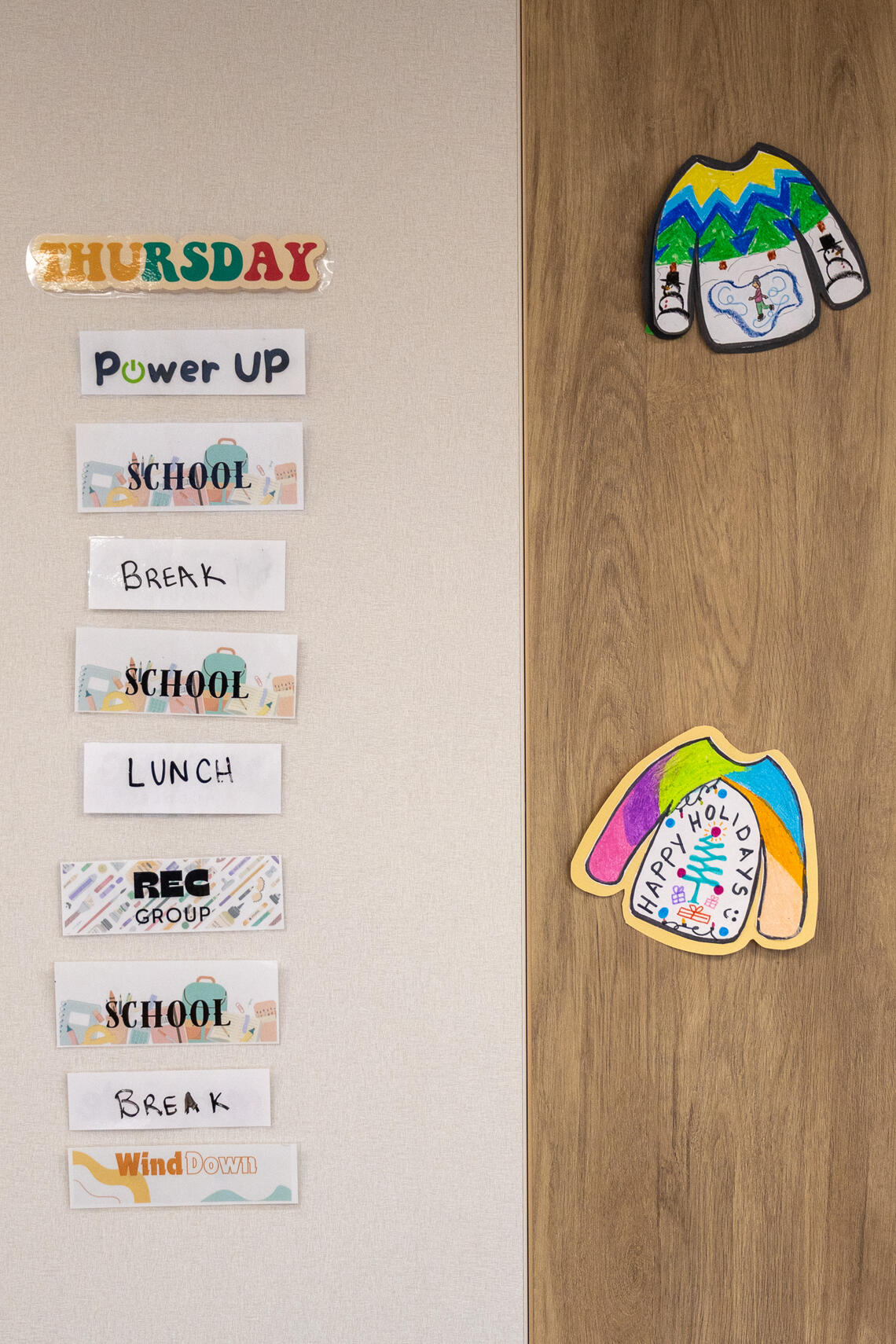
This unit was created with the goal of offering comprehensive care for youth facing complex challenges. The space is designed to feel safe and supportive, with customized rooms designed with safety in mind, a room for school and group activities, and a family room. The care team includes pediatricians, nurses, family counselors, an occupational therapist, a recreational therapist, a full-time teacher, and psychiatrists. This makes it one of only three units in Canada and the first of its kind in Alberta.
Dr. Carrah Bouma, MD, FRCPC, a Community Pediatrician, Clinical Assistant Professor, and the PLC Pediatrics Site Lead, was instrumental in its development. She shared, "This unit represents a significant step forward in providing comprehensive care for our youth. It’s a testament to our commitment to addressing both medical and mental health needs holistically."
Dr. Tyler Pirlot, the unit’s psychiatrist, also played a key role. His leadership in defining the unique patient population and mental health care protocols was critical. At its opening date, the unit was without a primary psychiatrist, he volunteered to step in, showing his dedication to this initiative and its youth.

PLC Unit 41 team
Unique Admission Criteria
What makes the Pediatric Med Psych Unit unique is its admission criteria. It’s designed for patients aged 6 to 17 who need a combination of medical and mental health care. To meet the criteria, patients must not require continuous monitoring or daily involvement from specialists. This focus allows the team to provide specialized care for both aspects of their inpatient treatment needs.
Thriving Together: A Collaborative Effort
The theme of "thriving together" underscores the unit’s operations, emphasizing collaboration between teams at the Alberta Children’s Hospital and PLC. This collaboration ensures patient’s needs are fully addressed. Staff members have undergone specialized training to provide integrated care for patients with combined medical and mental health needs.
The unit’s goal is to maintain full occupancy and improve communication with referring sources. The ultimate aim over time is to connect kids to outpatient services and reduce hospital readmissions. Dr. Bouma emphasized the importance of working as a team, saying, "We need to function together as a team, coming from very different training and leadership backgrounds. That’s the only way forward for our group to thrive together—or we won’t thrive at all."
Looking Ahead
The Pediatric Med Psych Unit at PLC, part of the Department of Pediatrics, sets a new standard for integrated care for youth with combined medical and mental health needs. Collaboration, specialized training, and a supportive environment are the foundation of its success.
Dr. Bouma expressed hope for the future, saying, "With appropriate funding and good resources, we could hone expertise and become the go-to resource for kids with these combined needs across the province."
This unit represents a big step forward for youth care in Alberta, offering compassionate, holistic support to help the next generation thrive.






Tina Sakon, TRACK Coordinator, Outreach Services, Alberta Children's Hospital
The METTA Clinic
Comprehensive Care for Transgender Youth
Clinic Overview and Services
Established in 2014 within the Endocrinology unit of the Alberta Children's Hospital (ACH), the METTA Clinic provides specialized care for transgender youth. The clinic's name “METTA” is derived from a Sanskrit term meaning "all-encompassing," chosen to offer privacy and inclusivity for families seeking care. Dr Danièle Pacaud, MD, FRCPC, a pediatric endocrinologist and Professor, explained that the clinic was created to address the unique needs of transgender youth through a multidisciplinary approach. The clinic's team currently includes endocrinologists, psychiatrists, adolescent medicine specialists, nurses, and a family therapist and social worker who work together to provide a safe environment for youth to explore their gender identity and receive appropriate medical care.

Dr. Daniele Pacaud

Dr. Daniele Pacaud
Patient Journey
When patients come to the METTA Clinic, they first undergo a mental health assessment with mental health professionals. This assessment process involves multiple sessions over one to two years to ensure the patient requires and is fit for medical interventions. Once the team determines that the patient is ready, they meet with an endocrinologist for a medical assessment and to discuss potential hormone therapies. The METTA clinic is the only one in the city that will prescribe hormone therapy to adolescents under the age of 16. Dr. Pacaud emphasized, "It's pretty amazing to see the transformation from a youth that comes in and is not well in their body and then see them transform into youth that can fully participate in all aspect of their adolescent life because they feel so much better as they go through their gender-affirming journey."
Challenges and Limitations
The clinic faces challenges, including long wait times for appointments, with some patients waiting 18 to 24 months to be seen. The clinic currently follows between 650 to 700 patients, with over 300 patients on the waitlist. Initially, the clinic started with only four physicians and no full-time therapists, seeing only one to two patients per month. Now, they receive 10 to 15 new referrals per month and a team of seven doctors, two nurses, one full-time social worker, and one family social worker. Dr. Pacaud remarked, "Of all the clinics I have been involved in, it's probably the one that is the most emotionally charged, but it's also probably one of the most rewarding because the families are so thankful to have the support we provide."
Thriving Together
The theme of "Thriving Together" is a fundamental aspect of the METTA Clinic's approach. The clinic operates as a multidisciplinary team, ensuring that youth receive assessments and support from various professionals. This collaborative environment allows for comprehensive care that addresses the unique needs of each patient. The clinic's partnerships with community organizations like Skipping Stone, the Calgary Sexual Health Centre, and the Calgary Board of Education further illustrate this. These collaborations provide a network of support that extends beyond the clinic, helping transgender youth and their families thrive in their communities. Dr. Pacaud emphasized the importance of this collective effort, noting that the transformative journeys of youth are a testament to the power of thriving together. "The families are very grateful for the support and the intervention that they're allowed to get when they come through our clinic," Dr. Pacaud added.

Dr. Daniele Pacaud

Dr. Daniele Pacaud

Dr. Daniele Pacaud
