Our lab utilizes cutting edge functional and structural brain imaging techniques to study people with epilepsy whose seizures cannot be adequately controlled with medication. Our research aims to help improve surgical outcome and increase quality of life.
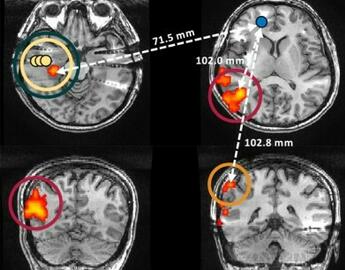
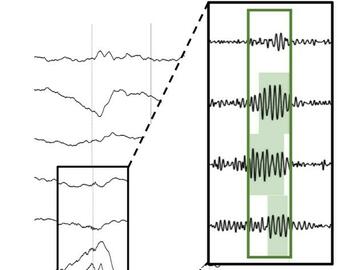
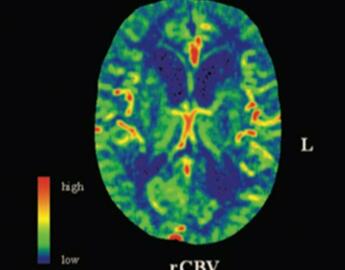
We are currently only one of two centres worldwide to utilize intracranial EEG-fMRI, a technique that combines the temporal accuracy of EEG with the spatial coverage of fMRI. We are also investigating novel interictal (between seizures) markers of seizure-generating tissue as well as exploring the physiological changes in the brain following a seizure.
Find out more about our research areas below.
We publish frequently in our areas of research. Click to view our publications