Alberta Perinatal Stroke Project (APSP)
Ongoing provincial collaborations are creating the largest population-based sample of perinatal stroke ever studied through the Alberta Perinatal Stroke Project (APSP). The rigorous collection of such patients will facilitate multiple institutional clinical and applied technology research programs. Examples include advanced neuroimaging studies to predict neurological outcome and understand plastic brain recovery. Another major focus is the identification of risk factors with dedicated studies examining clinical, placental, and biomarker risk profiles to better understand why strokes occur in the newborn period. Beginning in 2009, the APSP has identified >150 of an anticipated 700-800 children in Alberta currently living with perinatal stroke.

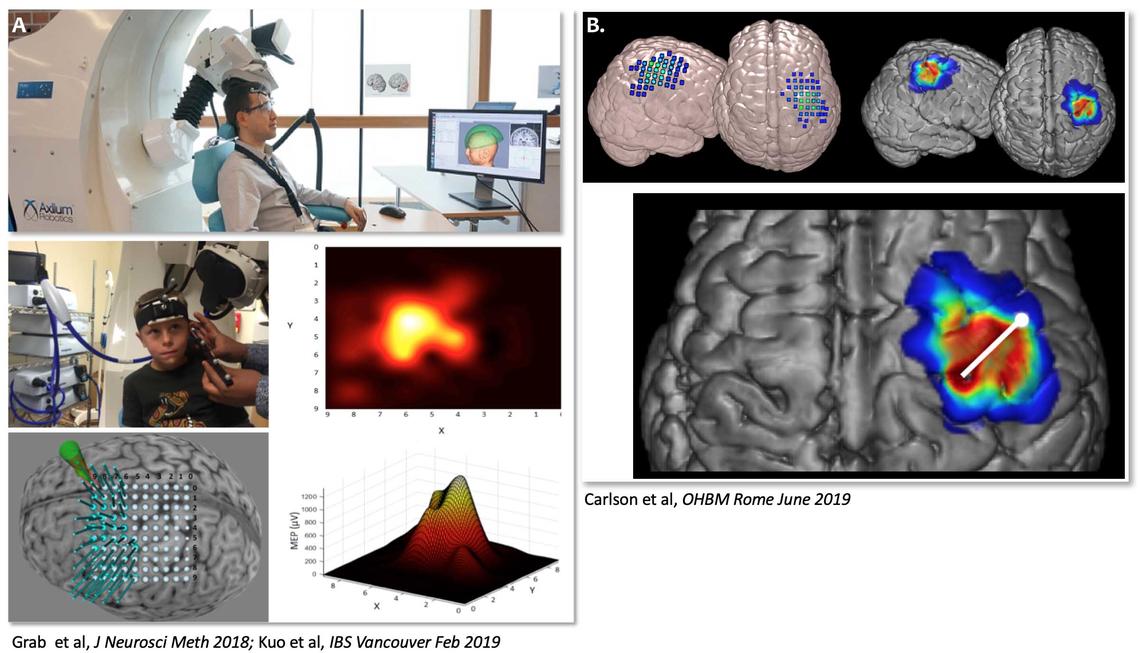
ACH Pediatric Transcranial Magnetic Stimulation (TMS) Laboratory
In 2010, under the direction of Dr. Adam Kirton, the CPSP opened the ACH Pediatric Transcranial Magnetic Stimulation (TMS) Laboratory. TMS technology has the remarkable capacity to both measure and “map” how a child’s brain recovers from injuries like stroke but also possesses a therapeutic potential with the possibility that repetitive TMS could help guide a child’s brain toward better recovery. Ours is the first TMS laboratory dedicated to children in Canada and one of only a few such facilities in the world. Ongoing studies are examining brain plasticity after stroke as well as other aspects of brain development and pediatric neurological disease. Funding to establish the lab was provided by community support through the Alberta Children’s Hospital Foundation.
Using the only pediatric TMS robot in the world, we can create personalized motor maps of individual hand muscles in the motor cortex. Robot-guided TMS with neuronavigated motor mapping provide unique, individualized representations of motor cortex neurophysiology. TMS maps can characterize both ipsi- and contralateral corticospinal tract configurations and cortical maps that are associated with motor function. Outcomes include peak hotspot locations, centre of gravity, and fractional areas and volumes of individual hand muscles. Maps can then be projected into standardized space to investigate neuroplastic changes and relationships to other imaging biomarkers. The white line in the image on the right represents a vector illustrating the magnitude and direction of displacement of primary motor cortex in an individual child after perinatal stroke compared to a standard location (white circle). Motor maps also provide targets for non-invasive brain stimulation in therapeutic intervention trials. Adrianna Giuffre, and Drs Ephrem Zewdie, Liu Shi Gan, James Wrightson and Helen Carlson are collaborating on these projects.

Brain Computer Interface (BCI) and Adaptive Technology Research
Electroencephalogram-based (EEG) brain computer interfaces (BCIs) are an exciting emerging technology that analyze and interpret electrical brain signals to turn them into simple commands for controlling an external application, such as accessing a communication device, turning on lights, or playing a computer game. Our talented research team is developing cutting-edge techniques to allow children with profound motor disabilities (for example, quadriplegic cerebral palsy) who have had limited success with existing access technologies to use BCI as a novel way to access play; including playing simple video games with their friends, driving remote control toys, and even painting pictures on a canvas.
The mission of the BCI program is to provide opportunity for children with severe neurological disability to access leading-edge, non-invasive brain computer interface technology to achieve greater independence and quality of life. The vision is to build and grow a child- and family-centred clinical program that connects emerging BCI technologies with affected patients while at the same time engaging patients to inform technological progress.
In parallel to the clinical program, our team of neuroscientists and biomedical engineers are working hard to further our understanding of pediatric BCI technology and implement state-of-the-art paradigms, signal processing techniques and applications specifically designed for pediatric BCI users.
Visit our website: BCI4Kids

Advanced Brain Neuroimaging
Magnetic resonance imaging (MRI) affords incredible opportunities to explore how brain structure and function change as children grow (developmental plasticity). We have used advanced imaging to demonstrate a broad array of brain differences after perinatal stroke. The resulting models have pioneered novel therapeutic neuromodulation strategies where imaging can also interrogate mechanisms of change (interventional plasticity).
We use MR modalities to explore differences in structural characteristics (lesion mapping, cortical thickness, gyrification, cortical and subcortical volumes, myelination mapping), functional connectivity, structural connectivity, and biochemistry between patients with perinatal stroke and typically developing peers. Using this information we hope to customize rehabilitation treatments to provide patient-centred customized care for each patient.
We are currently expanding to investigate functional near infrared spectroscopy (fNIRS) as a way to measure blood flow in the cortex without an MRI. This new technology will be more useful for investigating the motor networks in patient groups that cannot have an MRI such as toddlers.
Brandon Craig, Adrianna Giuffre, Jacquie Hodge, and Drs James Wrightson, Bryce Geeraert and Helen Carlson are collaborating on many many ongoing neuroimaging projects. For more specific information on our neuroimaging projects, please visit the Carlson Imaging Lab website.

Stimulation for Perinatal Stroke Optimizing Recovery Trajectories (SPORT) Trial
Perinatal stroke causes lifelong neurological disability and most hemiparetic cerebral palsy (CP). Effects of CP span many diverse aspects of a child’s life such as motor and cognitive domains and may lower quality of life. The SPORT trial is intended to investigate a new treatment for perinatal stroke, combining non-invasive neurostimulation and child-centred intensive rehabilitation. SPORT is a multicentre trial to explore whether this treatment can improve function in children with perinatal stroke and hemiparetic CP. The trial is the vision of Dr. Adam Kirton of the Calgary Pediatric Stroke Program at the Alberta Children's Hospital which is the lead site. Other sites include Toronto's Holland Bloorview Kids Rehabilitation Hospital and Edmonton's Glenrose Rehabilitation Hospital.
The SPORT camp is a fun, patient-centred summer day camp filled with activities such as baking and cooking, board games, crafts, one-on-one occupational and physical therapy, rock band gaming, swimming, soccer, tennis and mini golf. The social aspects of the camp are also exciting, children get to meet and hang out with other kids with similar physical disabilities and realize they are not alone. The last SPORT camps ended in Summer 2022, and all assessments were completed by March 2023.
SPORT participants and families are invited to sign up for a webinar to share study results here.
Participants and their families are invited to share their thoughts about the results in a separate study called “Enriching biomedical data interpretation: use of member-checking in the SPORT randomized controlled trial”. This study provides the opportunity for participant and family perspectives that might otherwise be missed by researchers. Participant feedback will help make sure the trial results and explanation of the results are meaningful. Participants and families will be asked to complete a short online survey, and if interested, complete a 30-60 minute online conversation with a researcher to share more thoughts. A link to join the study will be shared after the results webinars.

Modulation of Brain Plasticity After Perinatal Stroke: The PLASTIC CHAMPS TRIAL
This major CPSP study was funded by the Heart and Stroke Foundation of Alberta. PLASTIC CHAMPS was a clinical trial that tested the ability of two interventions - brain stimulation with TMS and constraint-induced movement therapy (CIMT) - to improve motor function in children with weakness after perinatal stroke. At the same time, TMS measured the changes that occurred in the brains of children undergoing such treatments.
More details of the study can be found here: PLASTIC CHAMPS Trial
A story about the study: Old therapy could help young patients
Results of the trial are published here: Kirton et al. (2016) Neurology

International Pediatric Stroke Study (IPSS)
The CPSP is an enrolling site in the International Pediatric Stroke Study (IPSS), a global research initiative in childhood stroke now spanning 135 centres in 35 countries. As of October 2010, the IPSS has enrolled >2400 children with stroke including many from Southern Alberta. The resulting studies now being published have greatly advanced the understanding of pediatric stroke in important ways. The CPSP is currently leading on several IPSS studies including several in the area of neonatal arterial ischemic stroke.
Multicentre Pediatric Stroke Studies
The CPSP currently participates in other multicentre pediatric stroke studies. These include a validation study of a pediatric version of the NIH Stroke Scale (PedNIHSS), the Vasculopathy and Infection in Pediatric Stroke (VIPS) study, and the Thrombolysis in Pediatric Stroke (TIPS) clinical trial, all funded by the National Institutes of Health. Additional multicentre studies are expected in the near future.
Additional Research Interests
The CPSP team is also conducting quality improvement research to better understand the educational and support needs of pediatric stroke families. Other areas of active research include imaging markers of acute brain changes (diaschisis) in newborns and children with stroke, the epidemiology of perinatal stroke syndromes, serum biomarkers of stroke pathophysiology in children with stroke, and the role of modifiable lifestyle risk factors (blood pressure, exercise, cholesterol) in secondary stroke prevention in children.
A list of current CPSP publications can be found here: PubMed

