Novel Risk Prediction Scores for ED Patients with Suspected Coronary Disease
This study has been approved by the University of Calgary Research Ethics Board (REB24-0536).
Help us make sure the right patient gets the right test at the right time.
PI: Dr. Andrew McRae
Co-PIs: Drs. James Andruchow, Jessalyn Holodinsky, and Tolulope Sajobi
Clinical Relevance:
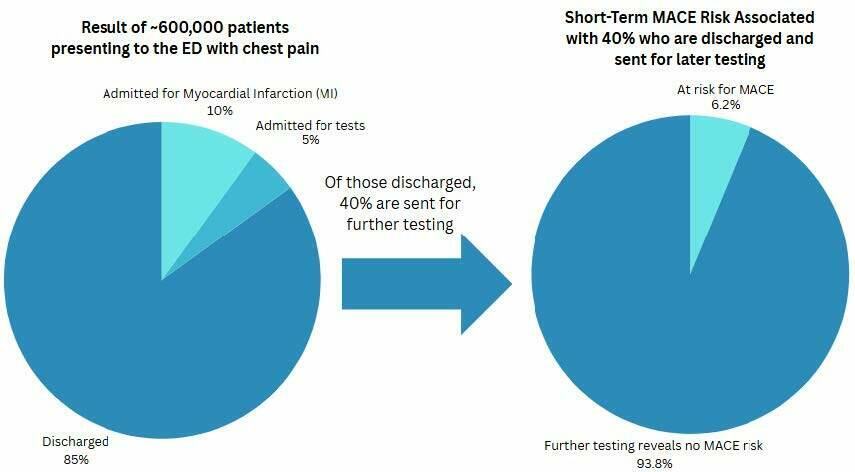
Each year, Canadian Emergency Departments (EDs) see over 600,000 patients with chest pain or other symptoms of coronary artery disease (CAD)1. Of these patients, only ~15% are diagnosed with myocardial infarction (MI, also known as a heart attack) or are admitted for further testing 2. The remaining 85% who have had MI and other high-risk diagnoses ruled out in the ED, have a short-term risk of Major Adverse Cardiac Events (MACE) being at 2.5% or less 3,4,5. Yet, over 40% or ~204,000 of these patients are sent for extensive outpatient testing each year to identify only 6.1% of patients at risk for MACE.
This is an ineffective use of healthcare resources.
Objective:
To derive, and internally validate, a novel risk prediction tool to accurately predict 30-day MACE among ED patients with chest pain in whom MI has been ruled out and who are considered for ED discharge. This risk prediction tool will guide rational, cost-effective decisions around which patients should be referred for additional cardiovascular testing after a thorough ED evaluation for chest pain. Even a modest 10% improvement in specificity of referral practices, while maintaining acceptable sensitivity, could safely translate to an annual reduction of over 50,000 unnecessary outpatient consultations and tests in Canada, thus improving access to care for patients with higher pre-test probability of coronary disease and reducing costs.
Background:
While referral to outpatient cardiology and/or testing has been associated with a 50% reduction in 1-year mortality and fewer re-hospitalizations, this phenomenon is likely due to poor clinical risk stratification6,7. Patients who are referred to outpatient cardiology tend to be younger, have fewer comorbidities, and a lower probability of coronary disease. In contrast, the patients who do not receive cardiology follow-up are older, have multiple comorbidities, and have a higher risk of all-cause mortality 6. This sort of over-referral for low-risk patients burdens the healthcare system and reduces access for higher-risk patients who are most likely to benefit from such tests.
There are several risk score assessments, including those created by Diamond and Forrster8,9, the HEART score, Manchester Acute Coronary Syndrome (MACS) Rule, Emergency Department Assessment of Chest pain Score (EDACS)10-14, and The Australian No Objective Testing Rule15. However, all the above assessments were created prior to the widespread availability of high-sensitivity cardiac troponin (hs-cTn) assays, which are now the gold standard15,16. They also do not account for differences in short-term MACE risk between male and female patients, who often present with different symptoms and severity17-21.
This study aims to prospectively develop a risk prediction tool to accurately estimate the risk of 30-day MACE in ED patients presenting with chest pain who are eligible for discharge after having MI ruled out. This will improve on existing tools in several ways:
- Developed on a contemporary Canadian patient population
- Patients are recruited AFTER MI is ruled out
- Improved accounting for sex-related MACE risk
- Use of high-sensitivity cardiac troponin assays
- Integration of multiple laboratory markers to enhance risk prediction
Methods:
Data is collected on patients in the EDs of academic hospitals across Canada:
- Calgary, AB: Foothills Medical Centre, South Health Campus, Rockyview General Hospital
- Vancouver, BC: Vancouver General Hospital, St. Paul’s Hospital
- Halifax, NS: QEII Health Sciences Centre
- London, ON: London Health Sciences Centre (University and Victoria Campuses)
- Kingston, ON: Kingston Health Services
- Toronto, ON: Sinai Health, Sunnybrook Research Institute
- Ottawa, ON: The Ottawa Hospital (Civic and General Campuses)
At most sites, patients will be recruited from 8am-8pm, 7 days/week while research staff are present. Eligible patients receive normal care provided by ED clinicians, including ECG and laboratory testing as per usual clinical practice. The eligible patients ED physician will fill out an online form with pertinent information for the creation of the risk assessment tool. This information includes the patient’s age, biological sex, gender, and clinical characteristics of their chest pain including the pattern, provoking and relieving factors, radiation locations, associated signs, risk factors, etc.
For patients to be eligible for the study, they must fulfill all the following inclusion criteria and must not fulfill any of the exclusion criteria, as seen below.
| Inclusion Criteria | Exclusion Criteria |
| 1. Symptoms of chest pain or of suspected cardiac ischemia (i.e. dyspnea, epigastric pain) undergoing ED evaluation for possible symptomatic coronary disease; | 1. Diagnosis of myocardial infarction made in the emergency department; OR any high-sensitivity troponin concentration >115ng/L; OR if second troponin measured, change between first and second troponin is >3ng/L AND >30% of the initial troponin concentration |
| 2. Age 25 or older; | 2. Acute ischemic ECG changes (ST segment elevation or depression, new T-wave inversion, New left bundle branch block; Wellen’s/DeWinter T waves); |
| 3. Alternative diagnosis identified in the ED (e.g. pneumonia, pulmonary embolism, aortic dissection, pancreatitis; peri/myocarditis); | |
| 4. Acute coronary syndrome or revascularization in previous 30 days; | |
| 5. Expected lifespan < 6 months per treating clinician. |
What do I need to do to get involved?
Think your patient might be eligible?
→ Click here to fill out a patient enrollment form or copy/paste this link into your browser: https://rc.med.ubc.ca/redcap/surveys/?s=MCCDJWXMDRFADE43
Patient Information:
If you present to a participating ED in Canada with chest pain or suspected cardiac ischemia, you may be enrolled into this study. Participants do not need to do anything to be enrolled.
References:
- Health Indicators Interactive Tool. Accessed February 9, 2023.
a. https://yourhealthsystem.cihi.ca/epub/?language=en - Bhuiya FA, Pitts LR, McCaig LF. Emergency department visits for chest pain and abdominal pain in the United States 1999-2008. NCHS Data Brief. Published online 2010.
- Scheuermeyer FX, Wong H, E Y. Development and validation of a prediction rule for early discharge of emergency department patients with potential ischemic chest pain. CJEM. 2014;16:106-119.
- Scheuermeyer FX, Innes G, E G. Safety and Efficiency of a chest pain diagnostic algorithm with selective outpatient stress testing for emergency department patients with potential ischemic chest pain. Ann Emerg Med. 2012;59:256-264.
- Andruchow JE, Kavsak PA, McRae AD. Contemporary Emergency Department Management of Patients with Chest Pain: A Concise Review and Guide for the High-Sensitivity Troponin Era. Can J Cardiol. 2018;34(2):98-108.
- Howarth A, Ji Y, B M. Chest pain clinic assessment after emergency department discharge with low risk chest pain is associated with a reduction in hospitalizations and emergency re-visitation. Circulation. 2016;134:A16257.
- Czarnecki A, Chong A, Lee DS, et al. Association between physician follow-up and outcomes of care after chest pain assessment in high-risk patients. Circulation. 2013;127(13):1386-1394.
- Diamond GA, Forrester JS. Analysis of probability in the clinical diagnosis of coronary artery disease. NEJM. 1979;300:1350-1358.
- Genders TSS, Steyerberg EW, H A. A clinical prediction rule for the diagnosis of coronary artery disease: validation, updating and extension. Eur Heart J. 2011;32:1316-1330.
- Backus BE, Six AJ, JC K. A prospective validation of the HEART score for chest pain patients at the emergency department. Int J Cardiol. 2013;168:2153-2158.
- Stopyra JP, Miller CD, BC H. Validation of the No Objective Testing Rule and Comparison to the HEART Pathway. Acad Emerg Med. 2017;24:1165-1168.
- Body R, Carley S, McDowell G, et al. The Manchester Acute Coronary Syndromes (MACS) decision rule for suspected cardiac chest pain: derivation and external validation. Heart. 2014;100(18):1462-1468.
- Body R, Carlton E, Sperrin M, et al. Troponin-only Manchester Acute Coronary Syndromes (TMACS) decision aid: single biomarker re-derivation and external validation in three cohorts. Emerg Med J. 2017;34(6):349-356.
- Than M, Flaws D, S S. Development and validation of the Emergency Department Assessment of Chest pain Score and 2h accelerated diagnostic protocol. Emerg Med Australas. 2014;26:33-44.
- Greenslade JH, Parsonage W, M T. A clinical decision rule to identify emergency department patients at low risk for acute coronary syndrome who do not need objective coronary artery disease testing: the No Objective Testing Rule. Ann Emerg Med. 2016;67:478-492.
- Gulati M, Levy PD, Mukherjee D, et al. 2021
AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines.
a.Circulation. 2021;144(22):e368-e454. - Sandoval Y, Bell MR, Gulati R. Transradial Artery Access Complications. Circ Cardiovasc Interv. 2019;12(11):e007386.
- Humphries KH, Lee MK, M I. Sex differences in diagnoses, treatment, and outcomes for emergency department patients with chest pain and elevated cardiac troponin. Acad Emerg Med. 2017;25:413-424.
- Hochman JS, Tamis JE, Thompson TD, et al. Sex, clinical presentation, and outcome in patients with acute coronary syndromes. Global Use of Strategies to Open Occluded Coronary Arteries in Acute Coronary Syndromes IIb Investigators. N Engl J Med. 1999 Jul 22;341(4):226-32.
- Ferry AV, Anand A, Strachan FE, et al. Presenting Symptoms in Men and Women Diagnosed With Myocardial Infarction Using Sex‐Specific Criteria. J Am Heart Assoc. 2019;8(17):e012307.
- Elsaesser A, Hamm CW. Acute coronary syndrome: the risk of being female. Circulation. 2004;109:565-567.

