
Family Medicine Clinical Experience Preceptor Information
All members of the care team extended a warm welcome and actively included me in the clinic processes and patient interactions. I immediately felt that this was a safe learning environment to ask questions and engage with the interdisciplinary team.
UofC Cumming School of Medicine Student - Class of 2023
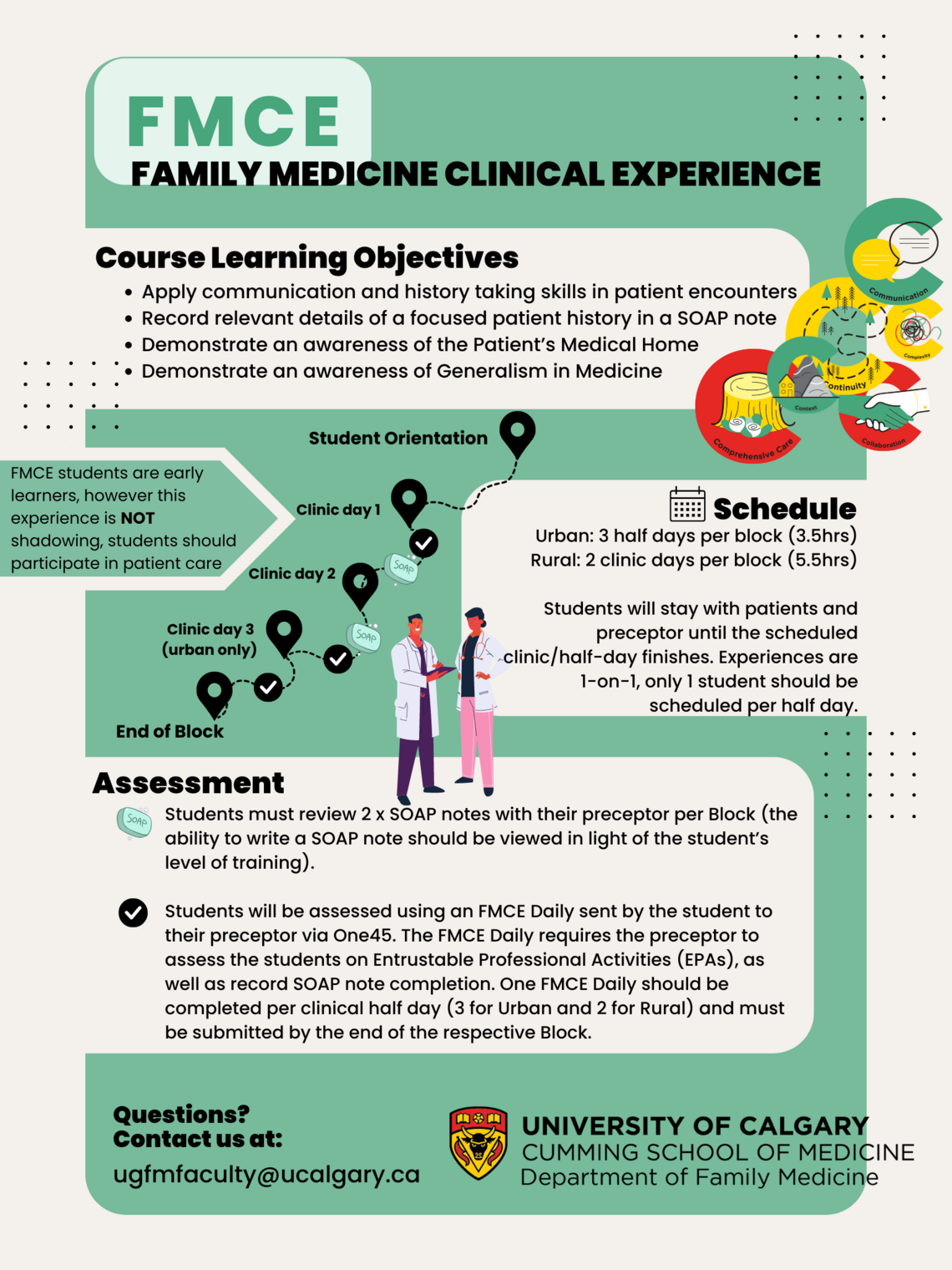
Family Medicine Clinical Experience (FMCE)
All of UofC first-year medical students will experience, and—with guidance— participate in the delivery of rural and urban Family Medicine across southern Alberta. Our preceptor physicians are skilled clinicians and educators who deliver community-based, generalist, continuity of care within a Patient’s Medical Home (PMH). Year over year, students highly rate the quality of preceptor teaching. This includes teaching and learning within safe and supportive environments, providing the right amount of guidance and autonomy for students to safely participate in care, and being approachable, non-judgmental and taking time to ensure meaningful student participation in patient care. It takes considerable preceptor skill to provide supportive educational experiences for our very early, engaged, and enthusiastic learners, ensuring student participation while concurrently delivering high quality, timely patient care.
Learning Objectives
All students will apply relevant office practice communication and history-taking skills identified in the longitudinal Clinical Skills course. Skills include introducing self to the patient and building rapport, identification of presenting complaint(s), and eliciting further relevant pertinent positive or negative information to help with assessment. Note that these further details are only expected if related clinical approaches and course work have been completed.
Skilled history taking will enquire and document biopsychosocial contexts (patient feelings, ideas, fears, and expectations) and social contexts (low literacy, poverty, or abusive environments).
Use of open and closed questions, attentive listening, recognition of verbal and non-verbal cues, avoidance of jargon and clarification are all applicable communication skills to apply.
In Clinic: To help with time management, chat with student/preceptor about expectations and time available to take the history prior to seeing patients.
History taking may be independent. If the student and preceptor initially choose to take histories together it is expected that this should progress to independent history taking with subsequent preceptor discussion. Preceptors and students may discuss the patient context prior to the visit; students may review medical records and related references before or after the visit. Students may accompany the preceptor in the exam room and participate in history taking, examinations, and discussions about diagnoses and planning. Students may also practice presenting the history verbally.
S Subjective
O Objective
A Assessment
P Plan
A SOAP note is written documentation to record the information and impression from a patient interaction. It should convey the information from an encounter that the writer feels is relevant for other healthcare professionals to provide appropriate care to the patient in the next encounter.
Subjective: Document the relevant history in Subjective. It is the STORY that you HEAR from the patient about their journey. Document the appropriate details you uncovered in your history- taking. With increasing experience students will organize by issue and prioritize issues.
Objective: Document relevant physical exam findings, vital signs, labs and investigations in Objective. This is what you MEASURE and OBSERVE. Ensure no history is recorded in Objective.
Assessment: Document what you think is going on in Assessment. It is your impression of the constellation of signs and symptoms before you.
Plan: Document what your course of action is to address each issue in Plan.
Both Assessment and Plan are informed by Subjective and Objective findings. We should consider when and why to return to care (continuity). At this early learner level preceptors most likely will have to make clinical reasoning overt to help learners understand how and why diagnoses and plans are developed.
As students progress through pre-clerkship RIME curriculum they are expected to incorporate more knowledge and practice more of their cumulative skills. There should be graduated responsibility based on student and preceptor comfort level after shared discussion of expectations for the clinic half-day.
In Clinic:
Review expectations that two (2) x SOAP notes are to be completed with preceptor review and feedback, one at the first clinic and another at a future clinic. SOAP notes without patient identifying data can be sent electronically if time is tight to review in clinic.
All physical examinations done by students must be with in-room physician (preceptor or Resident) or staff guidance and patient consent.
All students, whether in a rural or urban placement, must complete two (2) SOAP notes with preceptor review and feedback for each of Block 1 and Block 2 (i.e. 2 x SOAP notes per Block).
The Patient’s Medical Home is the evolution of family medicine in Canada. In this vision for primary care, every family practice across Canada will offer the medical care that Canadians want – readily accessible, centered on patients’ and families’ needs, throughout all stages of life, and integrated with other services in the community and health care system.
As students are placed into Patient’s Medical Home clinics, awareness may include discussions with preceptors about the PMH model of care, what makes a clinic a PMH, and any consideration of the 10 pillars. Awareness may also be demonstrated by including use of PMH health team members in SOAP note plans.
Watch the video.
Generalists are a specific set of physicians whose core abilities are characterized by broad scope of practice, able to respond to their patient and community needs. The Praxis of Generalism in Family Medicine involves the six (6) core concepts of (Kelly et al. 2021):
• Comprehensive Care
• Complexity
• Context
• Continuity of Care
• Collaboration
• Communication
These concepts will be both discussed and modelled in the Orientation and Midpoint sessions, the Small Groups, and in the Patient Medical Homes where you will have your clinical experiences.
Kelly, MA, Wicklum, S, Hubinette, M, and Power, L. 2021. The praxis of generalism in family medicine: Six concepts (6Cs) to inform teaching. Canadian Family Physician, 67 (10): 786- 788. DOI: https://doi.org/10.46747/cfp.6710786
FMCE Infographic
FMCE Infographic

