Common acne medication offers new treatment for MS
Multiple Sclerosis study results reveal safe and affordable option
A Canadian clinical trial led by researchers at the University of Calgary’s Hotchkiss Brain Institute (HBI), at the Cumming School of Medicine (CSM), shows that minocycline, a common acne medication, can slow the progress of relapsing-remitting multiple sclerosis (MS) in people who have recently experienced their first symptoms.
Press Release
In addition to being an unexpected discovery – an acne drug benefitting a neurological disorder – the discovery is significant as it offers a safe and affordable treatment option for those with early onset MS. This discovery could impact thousands of newly diagnosed MS patients around the world.
The results of the Phase 3 clinical trial will be published Thursday, June 1, 2017 in the New England Journal of Medicine. The trial included 142 participants between the ages of 18 and 60 across 12 Canadian sites including: Vancouver, Burnaby, Calgary, Edmonton, Winnipeg, Ottawa, Toronto, London, Montreal, Quebec City and Halifax.
MS is thought to be an autoimmune disease of the central nervous system (brain, spinal cord). The disease attacks myelin, the protective covering of the nerves, causing inflammation and often damaging the myelin. The drug works by reducing the inflammation.
In Canada, the cost of current therapies for relapsing-remitting MS typically falls in the range of $20,000 to $40,000 per year; the minocycline treatment would cost a fraction of that at about $600 per year. In the United States, MS treatment often costs about three times as much as in Canada. Researchers say the potential cost saving will be tremendous and will improve access to treatment for people with MS.
Researchers and doctors are excited about the discovery, as there are no oral therapies approved in Canada for use at this very early stage of the disease.
The drug itself has been around for 50 years, and it doesn’t need further Health Canada approval to be used as an off label prescription for MS.
“The clinical results are compelling,” says HBI member Dr. Luanne Metz, the study’s lead author, who is also a professor in the Department of Clinical Neurosciences at the CSM and an Alberta Health Services neurologist. “Based on these findings, neurologists will be able to prescribe minocycline for people experiencing their first symptoms of demyelination if an MRI suggests the cause will likely prove to be MS.”
“Patients will now have yet another treatment option, one that does not require injections, monitoring lab work, or special authorization by their insurance company provided they have adequate coverage to begin with. These processes can delay treatment initiation for three to four months whereas minocycline can be started immediately.”
Current care for many individuals experiencing a first clinical attack suggestive of relapsing-remitting MS involves a brain MRI at about six months to determine if MS can be confirmed or treatment with injectable medications to reduce the chance that their condition will evolve to confirm MS.
“We have not cured MS, but this trial makes future treatment easy and affordable. It has global impact because there are countries where people with MS cannot be treated because of the very high cost,” says V. Wee Yong, PhD, a study author from the HBI and professor in the Department of Clinical Neurosciences.
Jill, 34, experienced her first sign that she could be developing MS at 27. She woke up with tingling in her hand, the numbness spread to 50 per cent of her body before she received confirmation that lesions had formed on her brain and spine. She volunteered for the two-year clinical trial and kept taking the drug after the trial ended. “Joining the trial was an easy decision and the support I received throughout the process was excellent. I believe in research. How else are we going to learn?”
Jill is now symptom free and not been diagnosed with MS. After being on the drug for six years, Jill consulted with her physician and decided to stop taking the medication. “It is an antibiotic, and I wanted to give my body a break from all medication. I may go back on minocycline at some point. It’s great to have this option.”
The trial was funded by the Multiple Sclerosis Society of Canada and its affiliated Multiple Sclerosis Scientific Research Foundation (MSSRF). Participants in the trial who were experiencing their first demyelinating symptoms were randomized to receive 100 mg twice daily of the oral minocycline or placebo. Over six months of treatment, there was a 27.6 per cent reduction of becoming full blown MS. (The risk was 61 per cent in the placebo group and 33.4 percent in the minocycline group.) This is similar to the effects of current therapies.
“This is truly a Canadian success story in research that the MS Society of Canada and MSSRF are proud to be a part of,” says Dr. Karen Lee, vice president of research at the MS Society of Canada. “These are some of the world’s most experienced researchers and neurologists, who have taken an idea and brought it from bench to bedside. We are very encouraged by the results of the clinical trial and pleased that people living with MS will be provided a safe and beneficial treatment option as early in the disease as possible.”
This remarkable outcome for individuals experiencing demyelinating symptoms worldwide has been over 18 years in the making. Yong, a neuroscientist, initially had the idea to test the acne medicine in an animal model since minocycline has many anti-inflammatory properties that he thought could be useful in treating MS. Soon after obtaining successful research results, in studies also supported by the MS Society of Canada and MSSRF, Yong teamed up with Metz who led the transition into a pilot clinical trial, then a Phase 2, and finally the definitive Phase 3 trial. “This study highlights the benefits of evaluating existing therapies for other indications. Minocycline is an existing acne medication which is safe, and well-tolerated and it is available for immediate clinical use,” says Manitoba neurologist, Dr. Ruth Ann Marrie.
“Research has a profound impact on brain and mental health care. Drs. Yong and Metz have provided a remarkable example of how new brain health knowledge can be generated when the laboratory is bridged to the clinic,” says HBI Director Samuel Weiss, PhD. “This is a spectacular outcome that will positively impact people’s lives worldwide – and is a testament to the power of research excellence at the HBI and CSM.”
Led by the HBI, Brain and Mental Health is one of six strategic research themes guiding the University of Calgary toward its Eyes High goals.
The early stages of this work were supported by the Canadian Institutes of Health Research (CIHR) and community support. The clinical trial was supported by Multiple Sclerosis Society of Canada and the Multiple Sclerosis Scientific Research Foundation (MSSRF).
Media Contacts
Kelly Johnston
Senior Communications Specialist, Cumming School of Medicine
(403) 220-5012
kelly.johnston2@ucalgary.ca
Jennifer Asselin
Coordinator, MS Society of Canada
(1-800) 268-7582 ext. 3144
jennifer.asselin@mssociety.ca

In MS, immune cells (green) cross blood vessels (red) into the brain and spinal cord (the dark background) to mediate injury. Minocycline treatment reduces that influx and thus mitigates brain injury.
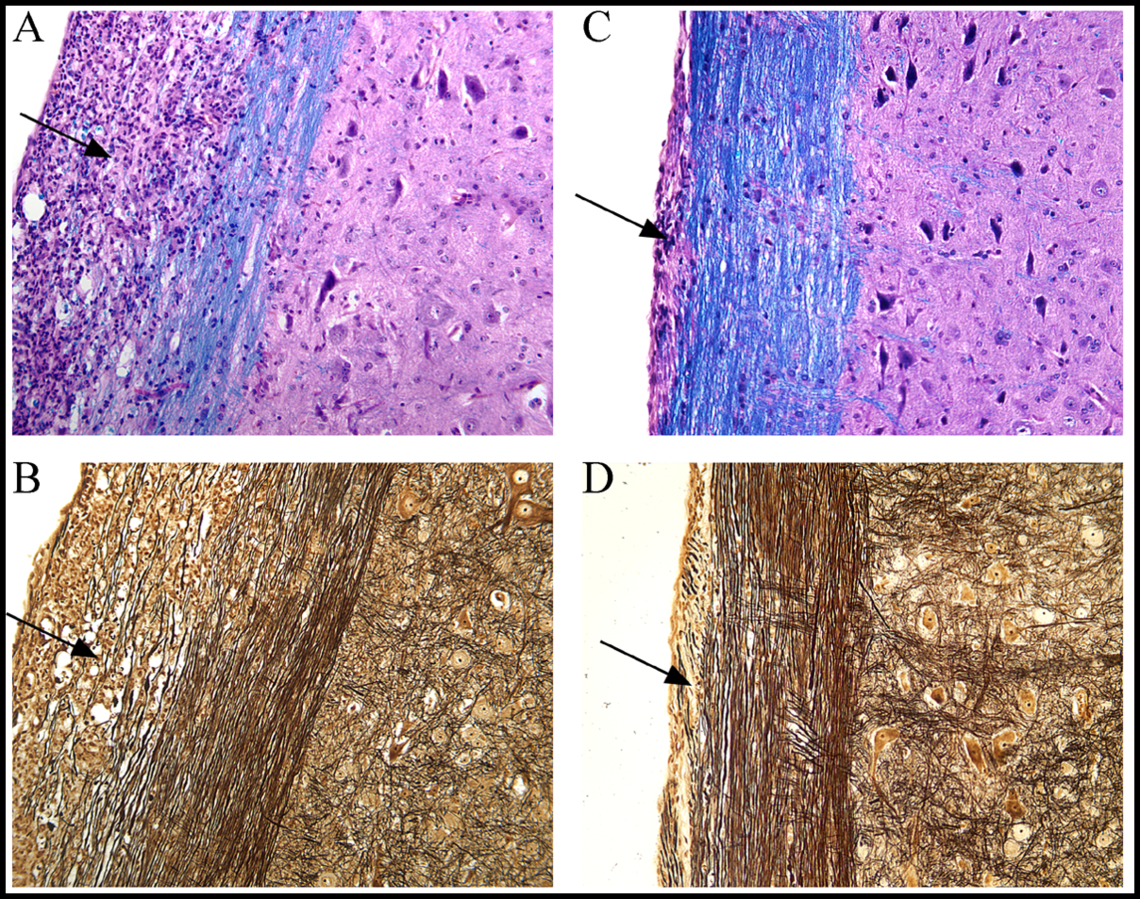
The inflammation (arrow in A), loss of myelin (blue stain) and nerve fibers (arrow in B) in the spinal cord of a model of MS is reduced by minocycline treatment (corresponding arrows in C and D).

Nerve fibers running lengthwise (left to right) in the spinal cord are disrupted by the MS disease process. This pathology is diminished by minocycline treatment.